Trauma, inflammation or frequent urinary tract infections can lead to a narrowing of one portion of the urethra, causing painful and obstructed urination. This kind of urinary blockage is called stricture, and it sometimes requires surgery.
What is reconstructive urology?
Reconstructive urology is surgery that helps patients with conditions such as cancer, birth defects, neurological disorders, male and female incontinence birth defects, stricture, scar tissue in the urinary tract organs and pelvic floor prolapse. It can also repair traumatic injuries to the ureter, kidney, bladder and genitals. Traumatic injuries are often associated with pelvic fractures that can happen as a result of things like car accidents or falls, and can often lead to scar tissue formation in the urethra.
Urologic conditions treated and reconstructive therapies offered at West Coast Urology includes:
- Bladder augmentation
- Bladder fistulas
- Bladder trauma
- Erectile dysfunction surgery
- Kidney trauma
- Penile trauma
- Surgical management of male and female urinary incontinence
- Testicular trauma
- Urethral stricture
- Urethral trauma
- Urinary diversion
What are the risks associated with reconstructive urology?
Although reconstructive urology has proven to be extremely safe, it poses potential risks and complications, as with every other surgical procedure. The safety and complication rates are similar when compared to open surgery, and potential risks include:
Infection All patients are treated with intravenous antibiotics prior to the surgery, to decrease the chances of an affection occurring after surgery. If an infection does occur, please contact us immediately.
Hernia Hernias at incision sites rarely occur since all keyhole incisions are closed carefully at the completion of your surgery.
Tissue or organ injury Tissue and organ injury is highly uncommon, possible injury to surrounding tissue and organs including bowel, vascular structures, spleen, liver, pancreas and gallbladder could require further surgery.
Bleeding Blood loss during this procedure is typically minor and a blood transfusion is rarely required.
Failure to correct UPJ obstruction
Almost 3 % of patients undergoing this operation will have persistent blockage due to recurrent scarring. If this occurs additional surgery may be necessary.
What to expect prior to the surgery
Once your surgical date is secured, you will receive a form along with a letter of explanation to take to your primary care physician or family doctor in order to have the following preoperative testing done prior to your surgery.
- Physical exam
- EKG (electrocardiogram)
- CBC (complete blood count)
- PT / PTT (blood coagulation profile)
- Comprehensive Metabolic Panel (blood chemistry profile)
- Urinalysis
Preparation for surgery
In preparation for your surgery, it is recommended that you avoid any medication that might cause bleeding during the surgery. These medication include aspirin, Motrin, ibuprofen, Advil, alka seltzer, vitamin E, ticlid, coumadin, lovenox, celebrex, voltaren, vioxx, plavix and some other arthritis medications.
It is also recommended that you do not eat or drink anything after midnight, and that you drink one bottle of magnesium citrate the evening before your surgery. Only drink clear liquids 24 hours prior to your surgery, as clear liquids can be seen through.
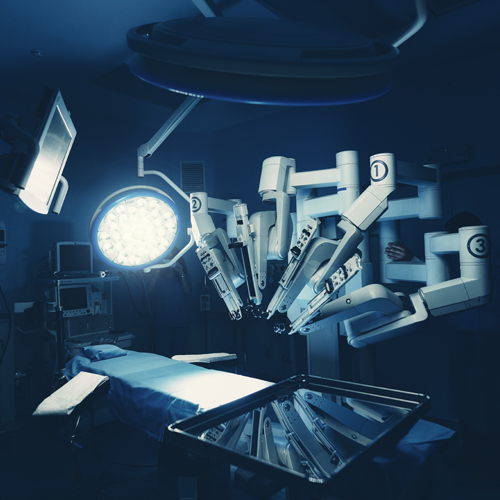
Surgery
Laparoscopic pyeloplasty is performed under a general anaesthetic. The typical length of the operation is 3-4 hours, and is performed through 3 small incisions made in the abdomen. A telescope and small instruments are inserted into the abdomen through these keyhole incisions, which allow the surgeon to repair the blockage or narrowing without having to place his hands into the abdomen.
A small plastic tube (called a ureteral stent) is left inside the ureter at the end of the procedure to bridge the pyeloplasty repair and help drain the kidney. This stent will remain in place for 4 weeks and is usually removed in the doctor's office. A small drain will also be left exiting your flank to drain away any fluid around the kidney and pyeloplasty repair.
Frequently Asked Questions with regards to reconstructive urology
-
How does the urethra become damaged?
-
How is stricture diagnosed?
There are different imaging techniques that can be used to identify stricture. A clinician might use dye and an X-ray to help identify the problem area using a technique called contrast imaging. In addition, an ultrasound helps to determine the exact stricture length prior to surgery. An endoscope or cystoscope (long, thin medical devices inserted inside the urethra) might also be used to identify the stricture.
-
How is reconstructive surgery performed?
Urethral reconstruction is a complex and delicate procedure, requiring several hours in the operating room and recovery time in the hospital. To repair the urethra, we will first identify the exact size and location of the blockage. Several different surgical procedures might be used depending on the extent of the stricture, the patient’s preferences, and overall health.